A Complete Guide To Testing During ACL Rehabilitation!
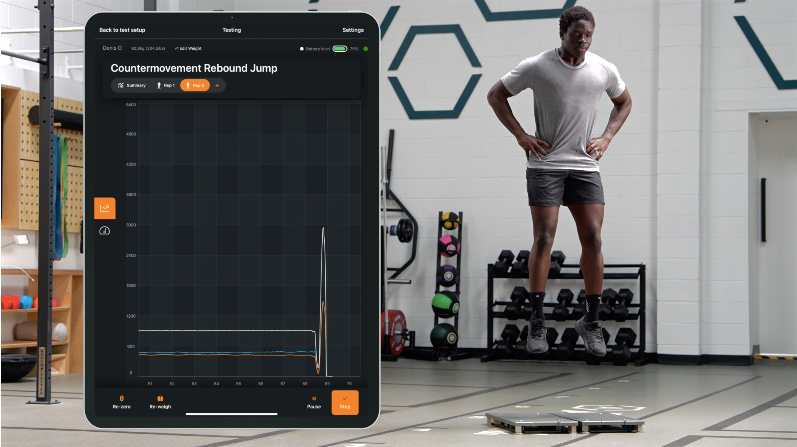
An Athlete Performing Jump & Hop Profiling on VALD ForceDecks
Following anterior cruciate ligament (ACL) reconstructive surgery, identifying the optimal timing for an athlete's return to sport is a crucial consideration. While the literature references both 9-month and 12-month 'time-based' return to sport guidelines, the 'criteria-based' return to sport strategy is now regarded as the most effective approach. We know that' “athletes who meet discharge criteria are six times more likely to return to pivoting sports compared with those who stop rehabilitation early" (1). It is therefore vital to work towards passing the criteria set at each rehabilitation phase.
Following ACL reconstruction, assessments should be conducted at regular intervals throughout rehabilitation, typically every 4–6 weeks. These reviews need not be limited to formal objective tests. Experienced sports physiotherapists and strength & conditioning coaches can obtain a reliable appraisal of progress by observing exercise performance in the gym. Training loads (for example, the weights being lifted) provide valuable, practical insight into how you are tracking physically, and help guide the adjustments required in your gym rehabilitation programme.
This article outlines the testing protocol used throughout ACL rehabilitation, culminating in the athlete meeting all return-to-sport criteria and resuming full athletic participation.
This Blog Will Answer The Following Questions
Why Is Testing Important?
What Tests Are Completed?
When Should I Complete Testing Throughout Rehabilitation?
What Should I Do With My Test Results?
What is The ACL Testing Protocol At Buan Physio?
ACL Profiling Timeline
-
This involves completing isokinetic knee flexion and extension testing, as well as jump and hop testing on ForceDecks, at approximately 4 months post-surgery.
-
This involves completing a comprehensive test battery, at approximately 6-7 months post-surgery. The results of profiling will help to guide what your training priorities will be for the forthcoming block.
-
This involves completing a comprehensive test battery, at approximately 9-12 months post-surgery. All tests must be passed in order to safely return to sport.
Profiling Session No.1
This normally occurs at 4 months post-surgery.
Testing should include the following :
Isokinetic Dynamometry
Knee Flexion & Knee Extension Strength
ForceDecks
2-Leg & 1-Leg Countermovement Jump
2-Leg Drop Jump
Strength Endurance
1-Leg Squat, Side Plank, 1-Leg Bridge, 1-Leg Calf Raise
Maximal Isometric Strength
Hip Joint
VALD ForceDecks
Profiling Session No.2
This normally occurs at 6-7 months post-surgery.
Testing should include the following :
Isokinetic Dynamometry
Knee Flexion & Knee Extension Strength
ForceDecks Testing
2-Leg & 1-Leg Countermovement Jump
2-Leg & 1-Leg Drop Jump
Quality of Movement Video Analysis / 3D Video Analysis
Deceleration Task
Unplanned 90-Degree Change of Direction
VALD Dynamo Isometric Testing
Profiling Session No.3
This normally occurs at 9-12 months post-surgery.
All tests should be passed in order to safely return to sport.
Testing should include the following :
Isokinetic Dynamometry
Knee Flexion & Knee Extension Strength
ForceDecks Testing
2-Leg & 1-Leg Countermovement Jump
2-Leg & 1-Leg Drop Jump
Quality of Movement Video Analysis / 3D Video Analysis
Deceleration Task
Unplanned 90-Degree Change of Direction
Maximal Dynamic Strength
5 repetition maximum testing for various compound lifts
Sports-Specific Physical Testing
Yo-Yo intermittent recovery test (aerobic & anaerobic system capacity)
10-30m acceleration
Maximal Velocity (using GPS Data)
Combined Neurocognitive & Motor Dual-Task Challenges
Neurocognitive Hop Test Battery
Field-based Neurocognitive Tests
Subjective Readiness Questionnaires
ACL-RSI Questionnaire (Psychological Readiness)
IKDC (Self-Reported Knee Function)
I-PRRS (Psychological Readiness)
5RM Strength Testing
Movement Quality Assessment Is A Critical but Frequently Overlooked Element of ACL Rehabilitation
Movement impairments are frequently observed following ACL surgery (15), making the restoration of movement quality critical during ACL rehabilitation (7). Video analysis is instrumental in determining how an athlete executes change of direction tasks. Despite individual movement variability, the evaluation focuses on whether the athlete aligns with an ideal technical movement model. This approach not only aids in reducing the risk of future injuries, but may also enhance performance.
"Restoring movement quality is a vitally important element of ACL rehab" (7)
Research has shown that reactive movements can adversely affect biomechanics, with varus/valgus and internal/external rotation moments being twice as high during unplanned cutting tasks, compared to pre-planned tasks (7, 14). Incorporating tests that include a reactive component (e.g. an unplanned change of direction) is therefore highly recommended, given the number of unplanned movements involved in sport.
ACL Testing Available At Buan Physio
VALD ForceDecks
VALD Dynamo
Video Analysis of On-Field / On-Court Movement Quality
5RM Strength Testing
NOTE : Your gym rehabilitation programme will be updated accordingly following each testing session. New agreed goals will be set in order to address any deficiencies identified.
Conclusion
A 'criteria-based' return to sport strategy is regarded as the most effective approach during ACL rehabilitation (1, 7). Adherence and progressing deep into the rehabilitation plan, along with completing on-field / on-court rehabilitation are keys to a successful outcome. There is no optimal or perfect testing procedure to determine one's readiness to return to sport (7), so we depend on the latest literature and expert consensus to inform decision making.
Restoring the neuromuscular elements that affect movement quality is a fundamental prerequisite before returning to sports. This process involves successfully passing isokinetic peak torque assessments for both the quadriceps and hamstrings, as well as restoring rate of force development (RFD), rapid maximal dynamic strength, heavy maximal dynamic strength and reactive strength. Return-to-sport evaluations should incorporate combined neurocognitive and motor dual-task challenges to assess the athlete's level of neurocognitive reliance. Additionally, it is essential for the athlete to reestablish their sport-specific fitness profile, in order to adequately prepare for the demands of competition.
Remember, you are six times more likely to return to pivoting sports by meeting your discharge criteria, compared to those athlete's who stop rehabilitation early (1). Returning to sport without fulfilling each criterion may also increase the risk of re-injury or other injuries.
If you are recovering from ACL surgery and you would like to organise a testing session, either email Declan at info@buanphysio.ie, or click on the button below to book online. Testing sessions are tailored to your current rehabilitation status and your specific requirements.
References
(1) Kotsifaki R, King E, Bahr R, et al. (2025). Is 9 months the sweet spot for male athletes to return to sport after anterior cruciate ligament reconstruction? British Journal of Sports Medicine. doi: 10.1136/bjsports-2024-108733
(2) Wilk KE, Arrigo CA, Davies GJ. Isokinetic Testing: Why it is More Important Today than Ever. IJSPT. 2024;19(4):374-380. doi:10.26603/001c.95038
(3) Santry Sport Clinic. ACL Reconstruction Rehabilitation Guidelines. Bone-Patellar Tendon-Bone (BPTB)
(4) O'Malley, E., Richter, C., King, E., Strike, S., Moran, K., Franklyn-Miller, A., & Moran, R. (2018). Countermovement Jump and Isokinetic Dynamometry as Measures of Rehabilitation Status After Anterior Cruciate Ligament Reconstruction. Journal of athletic training, 53(7), 687–695. https://doi.org/10.4085/1062-6050-480-16
(5) Zarro, M., Dickman, M., Hulett, T., Rowland, R., Larkins, D., Taylor, J., & Nelson, C. (2023). Hop to It! The Relationship Between Hop Tests and The Anterior Cruciate Ligament - Return to Sport Index After Anterior Cruciate Ligament Reconstruction in NCAA Division 1 Collegiate Athletes. International journal of sports physical therapy, 18(5), 1076–1084. https://doi.org/10.26603/001c.86130
(6) James, L. P., Talpey, S. W., Young, W. B., Geneau, M. C., Newton, R. U., & Gastin, P. B. (2023). Strength classification and diagnosis: Not all strength is created equal. Strength and Conditioning Journal, 45(3), 333-341.
(7) Buckthorpe M. (2019). Optimising the Late-Stage Rehabilitation and Return-to-Sport Training and Testing Process After ACL Reconstruction. Sports Medicine, 49(7), 1043–1058. https://doi.org/10.1007/s40279-019-01102-z
(8) van Melick, N., van Rijn, L., Nijhuis-van der Sanden, M. W. G., Hoogeboom, T. J., & van Cingel, R. E. H. (2019). Fatigue affects quality of movement more in ACL-reconstructed soccer players than in healthy soccer players. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 27(2), 549–555. https://doi.org/10.1007/s00167-018-5149-2
(9) Buckthorpe, M., & Roi, G. S. (2018). The time has come to incorporate a greater focus on rate of force development training in the sports injury rehabilitation process. Muscles, ligaments and tendons journal, 7(3), 435–441. https://doi.org/10.11138/mltj/2017.7.3.435
(10) Krosshaug, T., Nakamae, A., Boden, B. P., Engebretsen, L., Smith, G., Slauterbeck, J. R., Hewett, T. E., & Bahr, R. (2007). Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. The American journal of sports medicine, 35(3), 359–367. https://doi.org/10.1177/0363546506293899
(11) Buckthorpe, M., Pain, M. T., & Folland, J. P. (2014). Central fatigue contributes to the greater reductions in explosive than maximal strength with high-intensity fatigue. Experimental physiology, 99(7), 964–973. https://doi.org/10.1113/expphysiol.2013.075614
(12) Picinini, F., Della Villa, F., Tallent, J., Patterson, S. D., Galassi, L., Parigino, M., ... & Buckthorpe, M. (2025). High Return to Competition Rate After On-Field Rehabilitation in Competitive Male Soccer Players After ACL Reconstruction: GPS Tracking in 100 Consecutive Cases. Orthopaedic Journal of Sports Medicine, 13(3), 23259671251320093.
(13) Kotsifaki, R., Korakakis, V., King, E., Barbosa, O., Maree, D., Pantouveris, M., Bjerregaard, A., Luomajoki, J., Wilhelmsen, J., & Whiteley, R. (2023). Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. British journal of sports medicine, 57(9), 500–514. https://doi.org/10.1136/bjsports-2022-106158
(14) Besier, T. F., Lloyd, D. G., Ackland, T. R., & Cochrane, J. L. (2001). Anticipatory effects on knee joint loading during running and cutting maneuvers. Medicine and science in sports and exercise, 33(7), 1176–1181. https://doi.org/10.1097/00005768-200107000-00015
(15) Sterns KM, Pollard CD. Abnormal frontal plane knee mechanics during sidestep cutting in female soccer athletes after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2013;41(4):918–23.
(16) Grooms, D. R., Chaput, M., Simon, J. E., Criss, C. R., Myer, G. D., & Diekfuss, J. A. (2023). Combining Neurocognitive and Functional Tests to Improve Return-to-Sport Decisions Following ACL Reconstruction. The Journal of orthopaedic and sports physical therapy, 53(8), 415–419. https://doi.org/10.2519/jospt.2023.11489
(17) Labban, W., Manaseer, T., Golberg, E., Sommerfeldt, M., Nathanail, S., Dennett, L., Westover, L., & Beaupre, L. (2024). Jumping into recovery: A systematic review and meta-analysis of discriminatory and responsive force plate parameters in individuals following anterior cruciate ligament reconstruction during countermovement and drop jumps. Journal of experimental orthopaedics, 11(2), e12018. https://doi.org/10.1002/jeo2.12018
(18) Maffiuletti, N. A., Aagaard, P., Blazevich, A. J., Folland, J., Tillin, N., & Duchateau, J. (2016). Rate of force development: physiological and methodological considerations. European journal of applied physiology, 116(6), 1091–1116. https://doi.org/10.1007/s00421-016-3346-6